Anatomy: Liver and Gallbladder
|
|---|
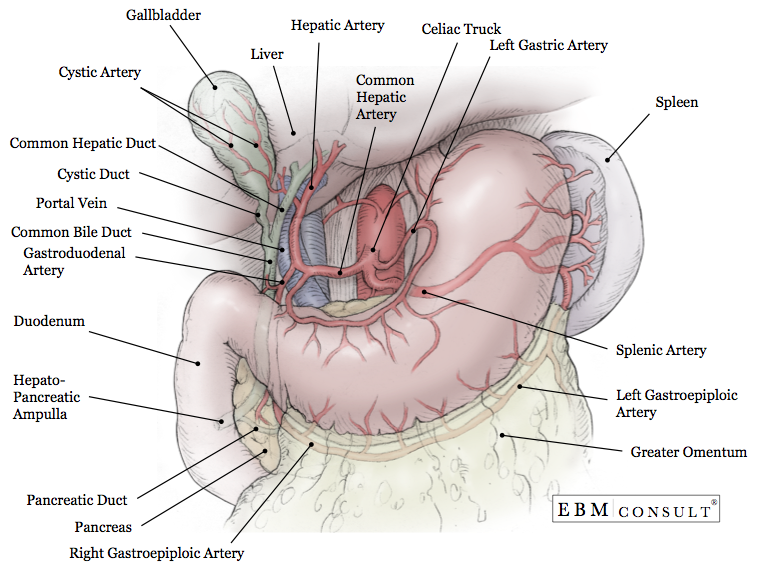
- Anatomy: Usually 5 - 15 cm in length and with a diameter usually < 4 mm. It is joined by the common hepatic duct coming from the liver and cystic duct coming from the gallbladder. It travels posteriorly, through the head of the pancreas to merge with the pancreatic duct and then onto the superior aspect of the duodenum to form the hepatopancreatic ampulla.
- Function: The distal end has circular smooth muscle to form the sphincter of Oddi to control the release of bile into the hepatopancreatic ampulla and then the duodenum. When closed it causes bile to back up into through the cystic duct to fill the gallbladder. Emptying of the bile from the gallbladder into the duodenum is controlled by fat entering into the intestines that causes the release to cholecystokinin.
- Blood Supply: Perfusion to proximal aspect is provided by the cystic artery, the middle aspect by the right hepatic artery, and the distal aspect by the posterior superior pancreaticoduodenal artery and gastroduodenal artery.
- Imaging: Best visualized by ultrasound
- Diseases: Ascending cholangitis, cholangiocarcinoma, cholidocholithiasis
- Clinical Considerations:
- Acute
Pancreatitis:
- Mu opioid agonists have been down to cause spasm or contractions of the circular smooth muscle at the Sphincter of Oddi which can prevent both bile and pancreatic enzymes from being secreted into the duodenum. In patients with acute pancreatitis, the use of parenteral opioids used to treat abdominal pain can actually worsen symptoms of pancreatitis if spasm of the sphincter occurs. Unfortunately, parenteral opioids are on the only appropriate analgesics while patients remain NPO (nothing by mouth).
- Anatomy: Formed after the merging of the right and left hepatic ducts. The common hepatic duct will eventually merge with the cystic duct to form the common bile duct.
- Function: Receive bile from the right and left hepatic ducts.
- Diseases: Cholangitis, cholangiocarcinoma
- Clinical Considerations:
- HIDA
Scan:
- Appropriate emptying of the biliary system can be assessed by a HIDA scan (or cholescintigraphy or hepatobiliary scintigraphy)
- Anatomy: 7 - 10 cm long structure that lies on visceral surface of the liver usually between the right lobe and quadrate lobe and anteriorly against the duodenum. The neck of is surrounded by the peritoneum helping to bind it to the liver.
- Components: Fundus, body, neck, cystic duct, common hepatic duct, common bile duct
- Normal wall thickness: On anterior view by ultrasound should be < 4 mm
- Function: Holds or stores up to 50 mL of bile to aid in the digestion of fat in the intestine. Emptying of the bile into the duodenum is controlled by fat entering into the intestines that causes the release to cholecystokinin, which causes contraction of the gallbladder.
- Blood Supply: Cystic artery. Cystic vein drains into portal vein.
- Innervation:
- Parasympathetic: Right phrenic nerve and vagus nerve
- Sympathetic: Greater splanchnic nerve and celiac ganglion and plexus
- Imaging: Ultrasound (preferred)
- Diseases: Cholecystitis, cholelithiasis, porcelain gallbladder
- Clinical Considerations:
- Murphy's Sign:
- Pain that is reported during full inspiration of the patient and while the provider applies direct pressure over the gallbladder in the right upper quadrant of the abdomen. The "Sonographic Murphy's Sign" is done with ultrasound probe instead of the provider applying pressure.
- Right
Upper Quadrant Pain:
- Pain especially after eating a high fat meal can be indicative of cholelithiasis. If this pain is associated with nausea and vomiting, fever, and/or an elevated WBC it can be concerning for the presence of acute appendicitis.
- Anatomy: Is a branch off of the celiac artery. The common hepatic artery comes directly off of the celiac trunk and then divides superiorly into the hepatic artery to perfuse the liver and gallbladder and then inferiorly as the gastroduodenal artery to perfuse a portion of the stomach and duodenum.
- Function: Provide the other 20 - 25% of blood flow to the liver. The cystic artery branches off the hepatic artery to perfuse the gallbladder.
- Variations: Abberrant hepatic arteries: The most common right aberrant hepatic artery comes off of the superior mesenteric artery and left aberrant hepatic artery comes off of the left gastric artery
- Anatomy: Continues to arise from the liver just inferior to the diaphragm.
- Function: Receives venous blood from the right, middle, and left hepatic veins of the liver and returns it to the right side of the heart for distribution to the lungs for oxygenation.
- Clinical Considerations:
- Vascular Status Assessment: Using ultrasound the IVC diameter and degree of collapse between inspiration and expiration can help to vascular status of the patient. A greater than 50% collapse can suggest volume depletion.
- Anatomy: Second to the skin, it is the largest gland in the body and weighs about 1,500 g. In children, it is about 5% vs. adults it is 2.5% of the body weight. It lies just inferior to the surface of right hemidiaphragm. It is divided into 2 main lobes and two accessory lobes that are created by reflections of the peritoneum. It is divided into 4 divisions and then further into 8 segments that can be surgically resected because each are independently perfused by branches of the portal triad.
- Ligamentum venosum: fibrous remnant of the fetal ductus venosus which was known to bypass the liver by shunting blood from the umbilical vein to the IVC.
- Round Ligament: is a fibrous remnant of the umbilical vein.
- Function: Its function is multifactorial:
- Receive nutrients from the gastrointestinal tract via the portal circulation
- Synthesize albumin, clotting factors, bile, and convert ammonia to blood urea nitrogen (BUN)
- Store glycogen and increase blood glucose levels via hepatogluconeogenesis
- Metabolize medications via phase I & II pathways
- Elimination of medications and bile into the bile canaliculus.
- Blood Supply: Hepatic artery and portal vein
- (Variations) Abberrant hepatic arteries: The most common right aberrant hepatic artery comes off of the superior mesenteric artery and left aberrant hepatic artery comes off of the left gastric artery
- Imaging: Ultrasound and CT scan
- Diseases: Cirrhosis, fatty liver disease, hepatocellular carcinoma, liver lacerations, abscesses
- Clinical Considerations:
- Cirrhosis:
- Fibrosis of the liver leading to loss of synthetic function as well as abnormal distribution and blood flow leading to portal hypertension. Numerous causes (alcoholic, alpha-1 antitrypsin deficiency, drug induced, fatty liver disease, hemochromatosis)
- Diabetes Mellitus:
- Patients with type 2 diabetes have insulin resistance that results in too much hepatogluconeogenesis. The oral medication, metformin works in the liver to reduce this process which improves fasting blood sugars.
- Liver Biopsy:
- Since the liver lies in the right upper quadrant and is protected in part by the overlying thoracic cage, the needle is commonly inserted in the right 10th intercostal space in the midaxillary line.
- Liver Laceration:
- Commonly from trauma or rib fracture. Can result in bleeding that may require surgical treatment.
- Subphrenic Abscesses:
- Normally collects from infections involving the peritoneal cavity such as ruptured duodenal ulcers and appendicitis that collect in the subphrenic recess.
- Traumatic
Intraabdominal Injuries:
- The large size in children in relation to adults puts children at greater risk for traumatic intrabdominal injuries.
- Tumor
Resection:
- Since each hepatic segment has its own blood supply, hepatic segmentectomies can be done to remove an isolate tumor.
- Anatomy: Formed by the inferior vena cava and the merging of the superior mesenteric and splenic veins. Enters the liver inferiorly.
- Function: Delivers about 80% of the blood supply to the liver and while less oxygenated that blood returning to the heart, still has sufficient amount of oxygen to oxygenate the haptocytes. The other portion of blood flow is from the hepatic artery.
- Imaging: Easily visualized by ultrasound
- Clinical Considerations:
- Portal Vein Thrombosis: venous thrombosis that can partially or fully occlude blood flow through the liver.
- Anatomy: Made up of the lesser omentum that surrounds the common bile duct (CBD), hepatic artery, and portal vein. It extends down between the lesser curvature of the stomach and the groove where the ligamentum venosum resides on the liver.
- Imaging: Beside visualized by ultrasound. A cross-section of this reveals the classic "Mickey Mouse" appearance with the portal vein making up the "head" and the CBD and hepatic artery making up the "ears".
- EBM Focused Topic: Enterolithotomy with or without Cholecystectomy for Gallstone Ileus
- Physical Exam: Murphy's Sign
- Ultrasound Reference Guide: Liver and Gallbladder (Hepatobiliary)
Common Bile Duct (CBD)
Common Hepatic Duct
Gallbladder
Hepatic Artery
Inferior Vena Cava
Liver
Portal Vein
Portal Triad
Related Content
MESH Terms & Keywords
|
|---|
|