Chronic pain syndromes are common in
patients with depression and have been associated with an increase in morbidity
and mortality.1,2 Clinicians are increasingly placed in scenarios
in which they must simultaneously treat both of these conditions.
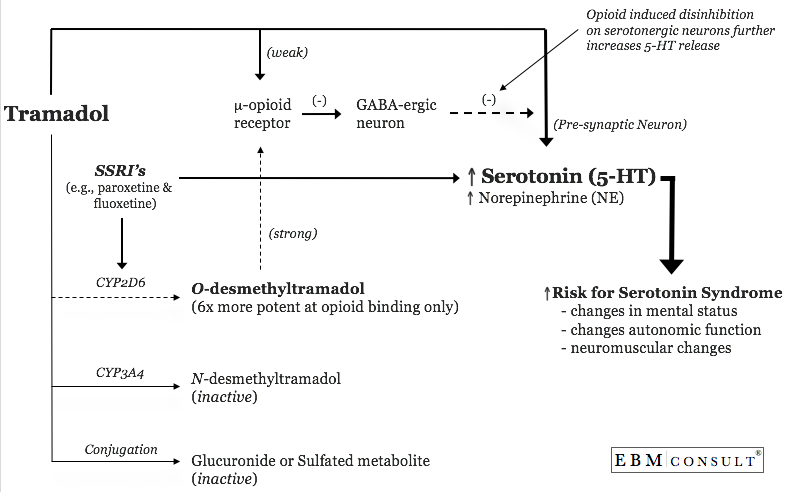
Tramadol (Ultram; Ultram ER; Ultracet) is a weak mu-opioid analgesic indicated
for the treatment of moderate to moderately severe chronic pain and has also
been recommended by some for pain patients with underlying depressive symptoms.3 Tramadol
may be useful in patients with underlying depressive symptoms because it is
also an inhibitor of the reuptake of the noradrenergic neurotransmitters
norepinephrine and serotonin.3 Tramadol's effects on these
neurotransmitters are dose dependent and have been shown to increase the risk
of seizures and serotonin syndrome.3,4
Serotonin
syndrome is often described as changes in mental status (e.g., agitation),
autonomic hyperactivity (e.g., diaphoresis, mydriasis, tachycardia, diarrhea)
and neuromuscular abnormalities (e.g., clonus, hyperreflexia).4,5 In
addition, it is important to recognize that this acute problem is not just an
idiopathic drug reaction, but rather a predictable consequence of excess
serotonin in the central nervous system (CNS), which produces a spectrum of
clinical manifestations ranging from barely predictable to lethal.4 The
risk of tramadol-induced serotonin syndrome increases with the use of higher
doses of tramadol, tramadol's opioid effect, concomitant use of medications
that inhibit the metabolism of tramadol and concomitant use of medications that
increase serotonin levels in the CNS. The last three causes are the focus
of the remainder of this issue.
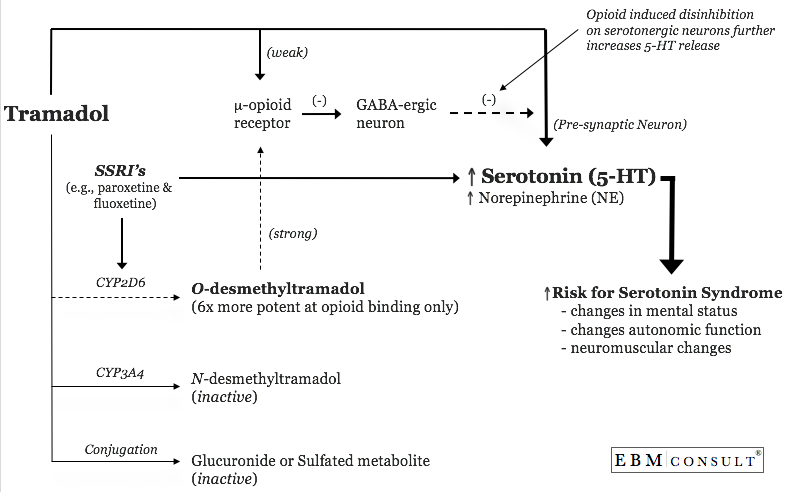
As
previously mentioned, patients with depression frequently experience chronic
pain that warrants treatment. It is therefore, very feasible that these
patients could receive tramadol for pain while also receiving a selective
serotonin reuptake inhibitor (SSRI) for depression.1,2 The problem with
the coadministration of these medications is two-fold. First, tramadol,
as well as all of the SSRI antidepressant medications (fluoxetine, paroxetine,
citalopram, etc), increase the concentration of serotonin in the synaptic cleft
of two connecting serotonergic neurons found in the midline raphe nuclei within
the brainstem. The neuronal pathways influenced by this include the
rostral end of this system, which is known to regulate affective behavior,
wakefulness, thermoregulation and food intake.4 In addition, the
serotonergic neurons of the raphe in the lower pons and medulla are known to
regulate nociception and motor tone.4 Lastly, serotonergic pathways in
the peripheral nervous system can influence vascular tone and gastrointestinal
motility.4 It is likely the influence of all of these neuronal pathways
that result in many of the classic symptoms seen in serotonin syndrome.
While there are 7 families of serotonin receptors (5-HT1 through 5-HT7), it
appears that excessive binding of serotonin to 5-HT2A and possibly to 5-HT1A
are the pathways most likely to result in the symptoms described above.6-9
This drug interaction is also supported by several case reports where an SSRI
(citalopram (10 mg/day), fluoxetine (20-80 mg/day), paroxetine (10-20 mg/day)
and sertraline (100 mg/day)) was given with tramadol 100-800 mg/day and the
combination resulted in the patient developing serotonin syndrome.10-16
The
second factor that may influence the development of serotonin syndrome is the
plasma concentration of tramadol. Tramadol is normally metabolized by
CYP2D6 and CYP3A4 enzymes to active and inactive metabolites.3 Therefore,
inhibitors of either enzyme will potentiate the effects of tramadol causing an
increase in the amount of norepinephrine and serotonin found in the synaptic
cleft. Several of the SSRIs (fluoxetine and paroxetine in particular) are
potent inhibitors of CYP2D6 and are likely to cause increases in tramadol
concentrations.3,17,18 As mentioned earlier, the risk of developing
serotonin syndrome while taking tramadol alone is notable and increases with
higher doses of the drug; this risk is compounded by coadministration of
SSRI's (specifically fluoxetine and paroxetine).3,17,18 As such, the manufacturer
of tramadol provides a bolded warning regarding this drug interaction.3
The
third influencing factor is ability of opioid medications to increase serotonin
release. This is not a direct effect of opioids but rather an indirect
effect. Opioids can also inhibit GABA-ergic neurons that are known to
decrease serotonin release.19,20 Therefore, opioids cause a disinhibition
that results in an increase in serotonin release.19,20